As humans have spread across the world, so have infectious diseases. Even in this modern era, outbreaks are nearly constant, though not every outbreak reaches pandemic level as COVID-19 has. Today’s visualization outlines some of history’s most deadly pandemics, from the Antonine Plague to the current COVID-19 event.
A Timeline of Historical Pandemics
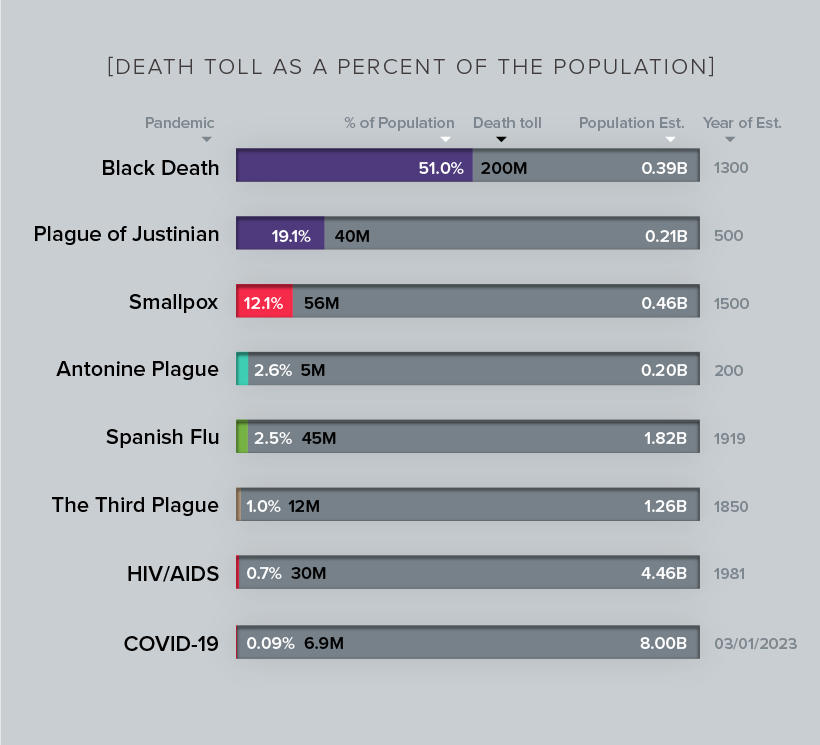
Disease and illnesses have plagued humanity since the earliest days, our mortal flaw. However, it was not until the marked shift to agrarian communities that the scale and spread of these diseases increased dramatically. Widespread trade created new opportunities for human and animal interactions that sped up such epidemics. Malaria, tuberculosis, leprosy, influenza, smallpox, and others first appeared during these early years. The more civilized humans became – with larger cities, more exotic trade routes, and increased contact with different populations of people, animals, and ecosystems – the more likely pandemics would occur. Here are some of the major pandemics that have occurred over time: Note: Many of the death toll numbers listed above are best estimates based on available research. Some, such as the Plague of Justinian and Swine Flu, are subject to debate based on new evidence. Despite the persistence of disease and pandemics throughout history, there’s one consistent trend over time – a gradual reduction in the death rate. Healthcare improvements and understanding the factors that incubate pandemics have been powerful tools in mitigating their impact. March 1, 2023 Update: Due to popular request, we’ve also visualized how the death tolls of each pandemic stack up as a share of total estimated global populations at the time.
Wrath of the Gods
In many ancient societies, people believed that spirits and gods inflicted disease and destruction upon those that deserved their wrath. This unscientific perception often led to disastrous responses that resulted in the deaths of thousands, if not millions. In the case of Justinian’s plague, the Byzantine historian Procopius of Caesarea traced the origins of the plague (the Yersinia pestis bacteria) to China and northeast India, via land and sea trade routes to Egypt where it entered the Byzantine Empire through Mediterranean ports. Despite his apparent knowledge of the role geography and trade played in this spread, Procopius laid blame for the outbreak on the Emperor Justinian, declaring him to be either a devil, or invoking God’s punishment for his evil ways. Some historians found that this event could have dashed Emperor Justinian’s efforts to reunite the Western and Eastern remnants of the Roman Empire, and marked the beginning of the Dark Ages. Luckily, humanity’s understanding of the causes of disease has improved, and this is resulting in a drastic improvement in the response to modern pandemics, albeit slow and incomplete.
Importing Disease
The practice of quarantine began during the 14th century, in an effort to protect coastal cities from plague epidemics. Cautious port authorities required ships arriving in Venice from infected ports to sit at anchor for 40 days before landing — the origin of the word quarantine from the Italian “quaranta giorni”, or 40 days. One of the first instances of relying on geography and statistical analysis was in mid-19th century London, during a cholera outbreak. In 1854, Dr. John Snow came to the conclusion that cholera was spreading via tainted water and decided to display neighborhood mortality data directly on a map. This method revealed a cluster of cases around a specific pump from which people were drawing their water from. While the interactions created through trade and urban life play a pivotal role, it is also the virulent nature of particular diseases that indicate the trajectory of a pandemic.
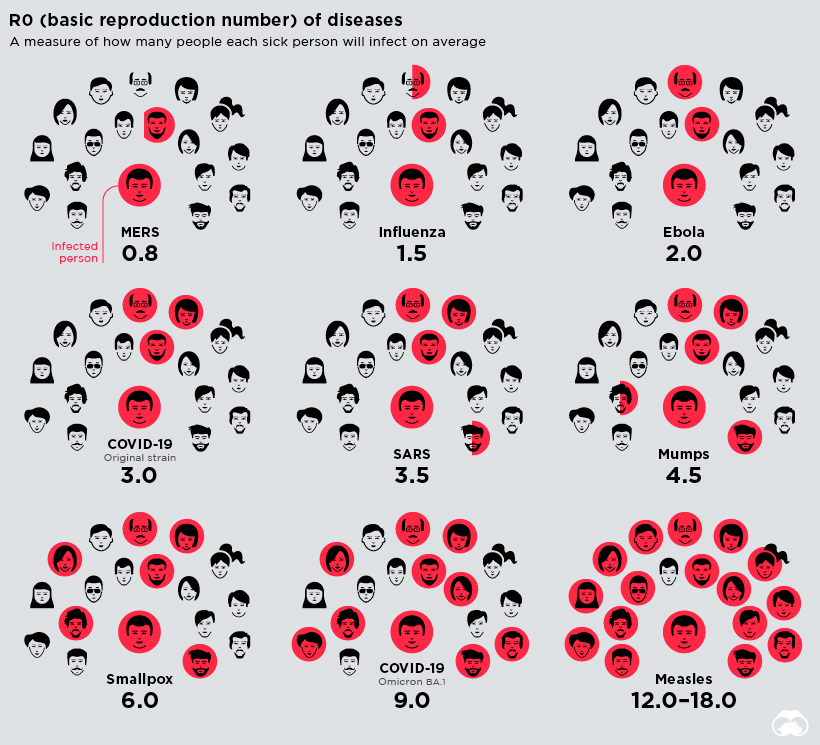
Tracking Infectiousness
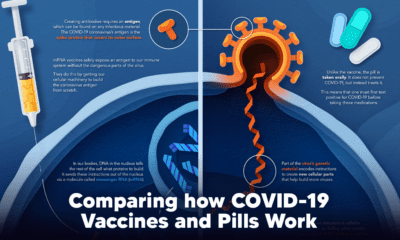
Scientists use a basic measure to track the infectiousness of a disease called the reproduction number — also known as R0 or “R naught.” This number tells us how many susceptible people, on average, each sick person will in turn infect.
Measles tops the list, being the most contagious with a R0 range of 12-18. This means a single person can infect, on average, 12 to 18 people in an unvaccinated population. While measles may be the most virulent, vaccination efforts and herd immunity can curb its spread. The more people are immune to a disease, the less likely it is to proliferate, making vaccinations critical to prevent the resurgence of known and treatable diseases. It’s hard to calculate and forecast the true impact of COVID-19, as the outbreak is still ongoing and researchers are still learning about this new form of coronavirus.
Urbanization and the Spread of Disease
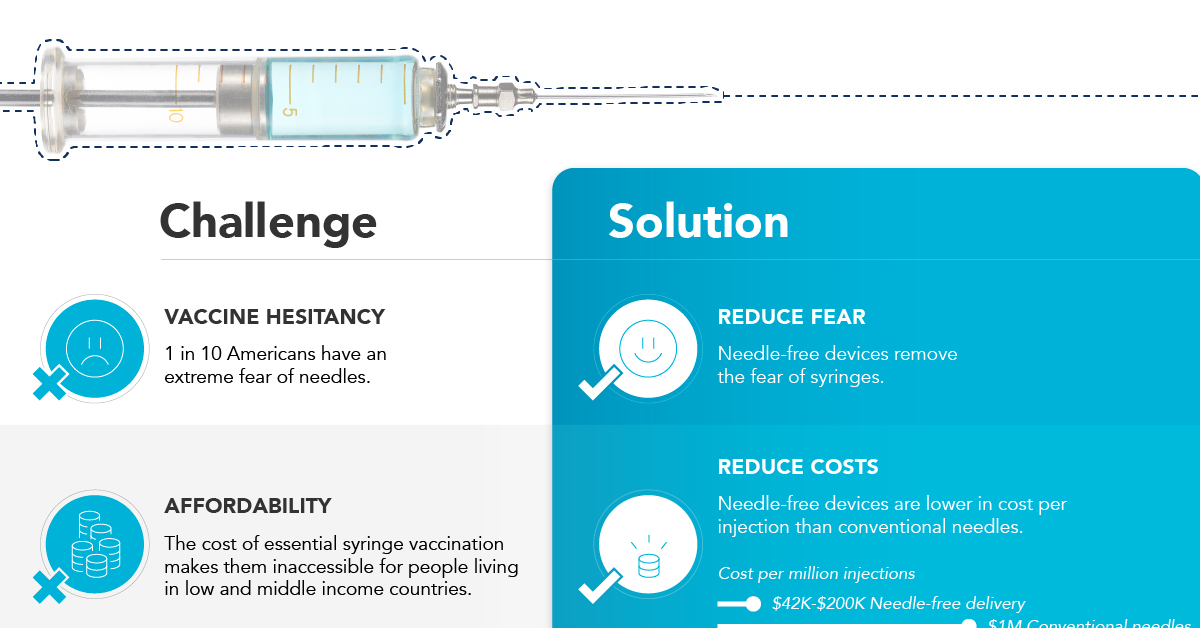
We arrive at where we began, with rising global connections and interactions as a driving force behind pandemics. From small hunting and gathering tribes to the metropolis, humanity’s reliance on one another has also sparked opportunities for disease to spread. Urbanization in the developing world is bringing more and more rural residents into denser neighborhoods, while population increases are putting greater pressure on the environment. At the same time, passenger air traffic nearly doubled in the past decade. These macro trends are having a profound impact on the spread of infectious disease. As organizations and governments around the world ask for citizens to practice social distancing to help reduce the rate of infection, the digital world is allowing people to maintain connections and commerce like never before. Editor’s Note: The COVID-19 pandemic is in its early stages and it is obviously impossible to predict its future impact. This post and infographic are meant to provide historical context, and we will continue to update it as time goes on to maintain its accuracy. Update (March 1, 2023): We’ve adjusted the death toll for COVID-19, and will continue to update on a regular basis. on In the above infographic from NuGen Medical Devices, we explore the factors leading to the syringe shortage and take a look at the company’s innovative needle-free solution that could play an important role in closing the immunization gap.
The Immunization Gap
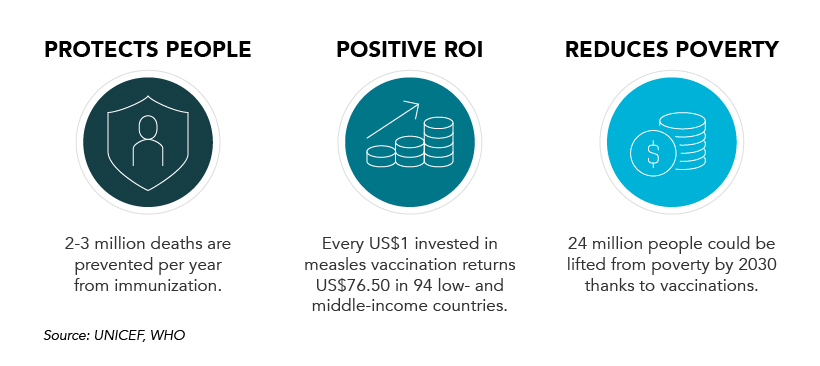
Even before the COVID-19 pandemic, millions of people around the world struggled to get access to routine vaccinations. In fact, as of 2019 more than 19 million children around the world were considered to be “zero-dose” which means that they did not receive any routine vaccinations. Moreover, when the COVID-19 pandemic hit, global immunization dropped even further with 25 million children missing out on routine vaccines in 2021 alone.
Why is Immunization So Important?
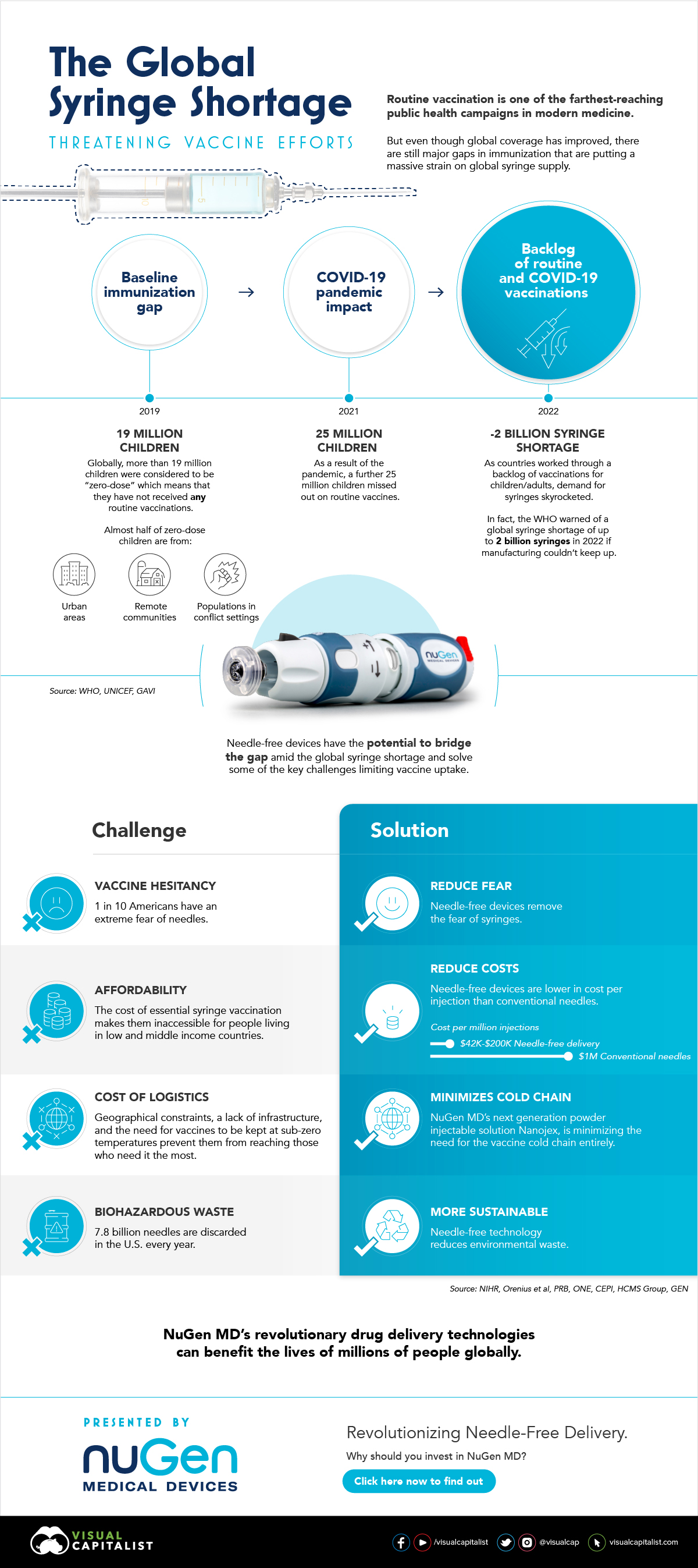
Vaccinations prevent against over 20 life-threatening diseases and save between 2-3 million deaths per year, making them—as the WHO describes—the foundation of healthcare systems and an indisputable human right. As countries work through a backlog of vaccinations to close the immunization gap that has worsened since the pandemic, demand for syringes has significantly increased.
The Result: A Global Syringe Deficit
In 2022, the WHO warned that we could see a shortage of up to 2 billion syringes if manufacturing can’t keep up. This could result in the severe disruption to routine vaccinations and promote unsafe recycling of syringes in order to administer vaccines. But the issue goes far beyond a supply shortage of syringes. COVID-19 has brought conventional syringe vaccines into sharp focus, with many criticizing the challenges associated with them. With conventional needles facing so many challenges, it’s no surprise that investors are taking interest in viable alternatives. What’s more, these alternatives don’t just apply to vaccinations, they can also work for people with diabetes, dentists, and pet care.
Enter Needle-free Devices from NuGen MD
Needle-free devices have the potential to bridge the gap in immunization amid the global syringe shortage, solve some of the key challenges limiting vaccine uptake, and more importantly, benefit the lives of millions of people.
How Do They Work?
NuGen’s needle-free devices use a simple spring-loaded mechanism which uses pressure to release the liquid drug and penetrate the skin. In less than one-tenth of a second, the drug is dispensed more safely and evenly compared to needle syringes. It’s also virtually painless and leaves no mark on the skin.
Interested in investing in NuGen Medical Devices? To learn more about their plans to pioneer the future of needle-free drug delivery, click this link now.